1. What is Schizophrenia?
2. What is Psychosis?
3. Why is Early Intervention important?
4. How do I get Help?
5. Why are Medications important?
6. Why has my loved one stopped taking their medication?
7. How can I tell the difference between symptoms versus side effects?
8. Are there different types of side effects?
If you have any questions that are not asked here, please contact us and we will try to help you find the answer you are looking for.
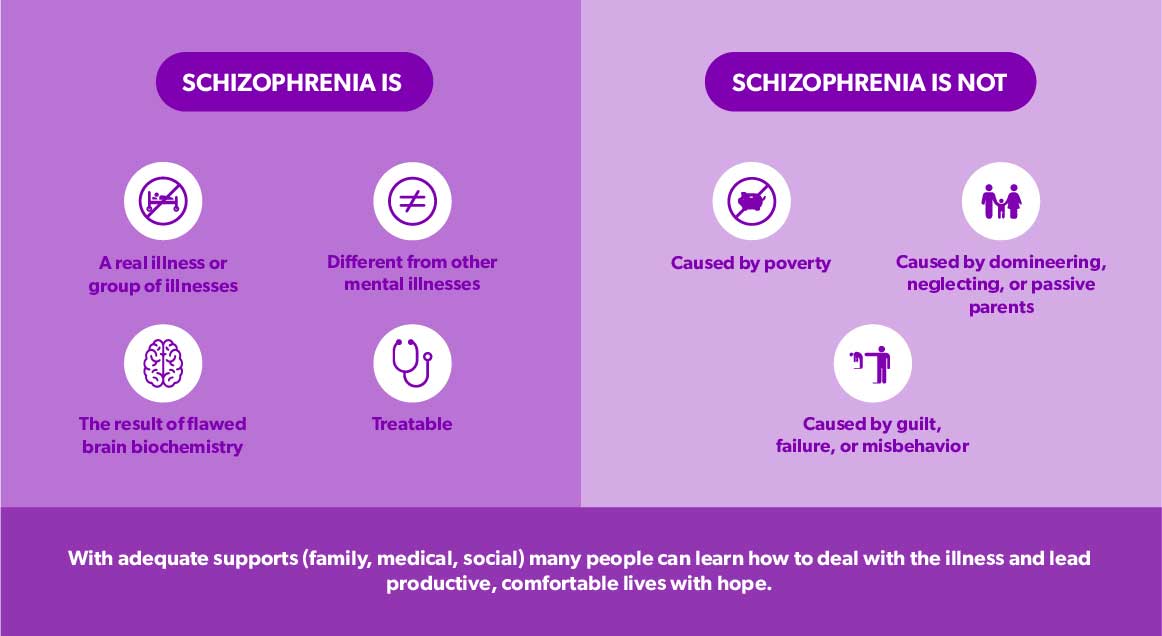
1. What is Schizophrenia?
Schizophrenia is an extremely complex mental illness that is different for everyone. Schizophrenia is a neurobiological illness, in the same cluster as Alzheimer’s, Parkinson’s, Temporal Lobe Epilepsy, Huntington’s, etc.
Schizophrenia is an illness that affects one’s sense of reality, it makes it difficult for the person affected to decide what is real and what is not real. It is characterized by a group of symptoms including hallucinations, delusions, disturbances of thinking, emotion, and behavior, and a deterioration of social functioning. Cognitive function is often severely affected. Schizophrenia affects a wide range of people spanning different races, cultures, and ages. Generally for males in their early 20’s and for women in their late 20’s to early 30’s.
2. What is Psychosis?
Psychosis is a word used to describe a collection of conditions that affect the mind and involve losing contact with reality. When someone becomes unwell or ill in this way it is often called a psychotic episode. Psychosis can include things like vivid hallucinations involving all five senses, delusions with are fixed false beliefs, paranoia, and many more. Psychosis can be a condition all on its own but can and often does present itself with schizophrenia, bipolar disorder, and even depression and anxiety in some cases.
Click here to view more symptoms of schizophrenia and tips for dealing with psychosis
3. Why is Early Intervention important?
There is evidence from early intervention studies that if you catch the signs of the symptoms early before a psychotic break and treat with medication immediately, that the person may never develop full-blown schizophrenia. Therefore, early recognition and timely intervention/treatment are the most important. Thus, it is imperative that school guidance counselors, youth workers, parents, and general practitioners have a keen awareness of the early warning signs of schizophrenia.
One of the difficulties of reading the early warning signs of schizophrenia is the easy confusion with some typical adolescent behavior. Schizophrenia can begin to affect an individual during the teen years, a time when many rapid physical, social, emotional, and behavioral changes normally occur.
If you have any concerns, the best course of action is to seek the advice of a trained mental health specialist. The following list of early warning signals of mental illness was developed by families affected by schizophrenia:
Most Common Signs
- Social withdrawal, isolation, and suspiciousness of others
- Deterioration and abandonment of personal hygiene
- Flat expressionless gaze
- Inability to express joy
- Inability to cry, or excessive crying
- Inappropriate laughter
- Excessive fatigue and sleepiness, or an inability to sleep at night(insomnia)
Other Signs
- Sudden shift in basic personality or behaviour
- Depression (intense and incessant)
- Deterioration of social relationships
- Inability to concentrate or cope with minor problems
- Indifference, even in highly important situations
- Dropping out of activities (and life in general)
- Unexpected hostility
- Hyperactivity or inactivity, or alternating between the two
- Extreme religiousness or preoccupation with the occult
- Drug or alcohol abuse
- Forgetfulness and loss of valuable possessions
- Unusual sensitivity to stimuli (noise, light, colour)
- Extreme devastation from peer or family disapproval
- Noticeable and rapid weight loss
- Attempts to escape through geographic change; frequent moves or hitch-hiking trips
- Excessive writing (or childlike printing) without apparent meaning
- Irrational statements
- Refusal to touch persons or objects; insulation of hands with paper, gloves, etc.
- Self-harm; threats of self-harm
- Staring, not blinking, or blinking incessantly
- Rigid stubbornness
- Peculiar use of words or language structure
- Sensitivity and irritability when touched by others
None of these signs by themselves indicate the presence of mental illness. Families who helped compile this list have indicated that they, unfortunately, had not acted on these early warning signs. With the benefit of hindsight and today’s knowledge about early intervention, family members are urged to seriously consider seeking medical advice if several of the behaviors listed above are present, or constitute a marked change from previous behavior, and persist over a few weeks.
4. How do I get Help?
Finding or asking for help can often be difficult, but it can be one of the bravest and most beneficial steps you can take for yourself or a loved one. Communicating with your family doctor about what is going on is often the best place to start. They are the ones that can refer you to psychiatrists, psychologists, and counselors for diagnosis, medication, counseling, and more. For an individual that may seem like too large of a jump, start by talking with a close family member, friend, or trusted adult. You will find that the more you open up to individuals you trust the easier it will get and the better you will feel. If you are searching for a family doctor accepting patients, this website may help you locate a clinic.
You may be tempted to search for information online using “Dr. Google”, but this is a mistake. A trained professional like a psychiatrist or psychologist are the ones who can help give a name to what might be going on.
5. Why are Medications important?
Although schizophrenia is not yet a “curable” illness, it is TREATABLE. The proper treatment includes the following four stepping stones to recovery:
- Medication to lessen symptoms and prevent relapse.
- Psychosocial rehabilitation helps men and women reintegrate into the community and regain social, educational, and occupational functioning.
- Psychoeducation for individuals and families to help solve problems, deal with stress, triggers, and cope with the illness and its complications.
- Empowerment and Recovery training to deal with the loss of sense of self and to deal with the various traumas associated with schizophrenia.
There are two categories of medications:
- Typicals – These are the older or “standard” antipsychotics introduced in the 1950’s include: Chlorpromazine (Largactil), Flupenthixol (Fluanxol), Fluphenazine (Modecate), Zuclopenthixol (Clopixol), Loxapine (Loxapac), Haloperidol (Haldol), Pimozide (Orap), Thioridazine (Mellaril), Trifluoperazine (Stelazine), Methotrimeprazine (Nozinan).
- Atypicals – These newer antipsychotics began to be introduced in the 1990’s. The following atypicals were available by the end of 1990’s: Risperidone (Risperdal), Olanzapine (Zyprexa), Clozapine (Clozaril), and Quetiapine (Seroquel).
The atypical antipsychotic medications have less severe (though still unpleasant) side effects, and work on negative as well as the positive symptoms. Often, with the older drugs, an individual had to take a second drug to control the side effects such as muscle rigidity, tremors, and involuntary movements. Side effects from the newer medications may be nasal congestion, obsessive-compulsive symptoms, and impaired glucose tolerance. Side effects can cause an ill person to be reluctant to continue with the medication. Ask your doctor or pharmacist for complete information on all medications.
6. Why has my loved one stopped taking their medication?
The most common reason for people to stop taking medication is that they don’t understand its importance, they lack insight into their illness, and/or are very suspicious that the medication may do them harm. The next most significant reason is the side effects of the medicines themselves. Side effects cause different levels of discomfort and vary highly from person to person.
Although medications can have great effects, they all come with some risks. This is called the medication’s safety profile. Prescribers must sometimes balance the positive effect of medication against any possible harm it might cause. Everyone responds differently to various medicines, so several may be tried to see which is the most effective with the fewest side effects. Psychotropic medications are relatively safe. However, the safety of their use also assumes that:
- A proper diagnosis has been made.
- Other medical conditions that could contribute to or imitate mental illness have been identified, treated, or ruled out.
- Proper medical follow-up is being done.
7. How can I tell the difference between symptoms versus side effects?
It is unlikely that someone will confuse hallucinations and delusions with side effects. However, other symptoms, such as ambivalence, avoiding people, problems with organizing thoughts, or feeling emotionally flat, may be harder to characterize. While some of these feelings and behaviours could be medication-related, they may also be negative symptoms, of psychosis. This means something that used to be there and no longer is.
Keep diligent notes of behaviours and changes. Inform your treatment team; especially the professionals involved with monitoring your medications.
The following groups are key behaviors or signs to look for and report to your treatment team. These may or may not be caused by your medication.
- Movement irregularities – These could include extrapyramidal symptoms (ESP) such as muscle spasms or stiffness, slow or exaggerated movements, twitches, and facial tics.
- Sleep or appetite disturbances – Any extreme change in behaviour for sleeping or eating patterns from too much to too little, a sudden change in your usual sleep/wake cycle or appetite, and fixations about certain types of food (color, smell, etc).
- Sexual issues – Either inability to have sex or an unusual change in the level of desire, problems with or a lack of menstruation, male or female breast engorgement, and dripping.
- Mood problems – Feeling agitated and restless, acting out aggression (throwing things, slamming doors, hitting), verbal abuse (screaming, cursing), and erratic driving.
- Thinking problems – Being unable to change focus (saying the same phrase over and over or constantly repeating the same action).
- Body changes – Weight gain or loss, constipation, problems urinating, dry mouth or nose bleeds, unexplained changes in vision or hearing, upset stomach, skin rashes, ears ringing, pounding headaches, a racing heart rate, feeling light-headed, and breathlessness.
That’s why these medications must be ordered and monitored by a prescribing specialist, usually a psychiatrist. Some medications have mild side effects that often go away in a short period of time. However, more serious long-term side effects are possible.
8. Are there different types of side effects?
Absolutely, the most common side effects for psychotropic medications are grouped into anticholinergic effects and extrapyramidal symptoms (EPS).
Anticholinergic Effects
Anticholinergic effects are caused when a medication interferes with acetylcholine, one of the chemicals the body makes to help nerve cells communicate with each other. Muscles and glands may be affected.
Anticholinergic effects may include:
- Confusion
- Blurred vision
- Constipation
- Dry mouth and nasal passages
- Light-headedness
- Difficulty with urination
- Problems with bladder control
- Palpitations
Sometimes these effects lessen as the body adjusts to the psychotropic medication. Many can be managed with small adjustments to the dose. Other nonmedical management methods can include sucking on hard candies for dry mouth or adding more fiber to your diet to relieve constipation.
Extrapyramidal Symptoms (EPS)
There is a network of nerve pathways in the brain known as the extrapyramidal system. This influences messages sent from the brain to the muscles. Certain medications – usually older types of antipsychotics – may disturb this system.
This can lead to:
- Involuntary movements such as tremors, writhing movements, rigidity, and jerking motions
- Problems with muscle tone and making the desired movements – such as slowed movement and rigidity seen with Parkinson’s disease.
- Many consumers do not develop EPS. For those who do, adjusting the medication dosage may solve the problem. If the problem continues, the prescriber may change to another medication or add another medication.
The newer antipsychotics have far fewer problems with EPS. As these medications become more common in the treatment of psychosis, EPS may become a less frequent problem. Another possible side effect involving the extrapyramidal system is called tardive dyskinesia (TD). This is much rarer than the EPS symptoms discussed above. It is not yet known whether the newer atypical products have a lower potential to cause TD. However, there is some research that suggests this may be the case.
Other Side Effects
A rare but serious side effect is neuroleptic malignant syndrome. This involves unusual muscle rigidity and elevated body temperatures. Vital signs may be unstable, and the person may drift in and out of consciousness. If a person has these symptoms, seek immediate medical attention.
As discussed earlier, side effects related to hormone changes can include breast enlargement, fluid discharge, impotence, and other sexual problems. There are fewer of these problems with the newer medications. Some consumers may become light-headed or feel dizzy when they get up from lying down. This is called postural or orthostatic hypotension. Usually getting up slowly and sitting on the edge of the bed for a moment or so before standing can help it.
Early intervention may prevent or lessen these and other serious side effects. Let your treatment team know if you have any problems that might be related to your medication. Also, the diaries and records you keep can help your treatment team see both your progress and problems.
If you have any questions that are not asked here, please contact us and we will try to help you find the answer you are looking for.